Yoga Therapy: The Newest Health Trend that Doctors are Paying Attention To
/Wellness enthusiasts have long known the healing benefits of yoga. However, the popularity of this ancient practice is now growing among today’s mainstream, especially doctors. Today, there is a rise in doctor-prescribed yoga therapy, even among Western-trained doctors.
So what is yoga therapy? Why is it a growing trend? Will yoga therapy help patients feel better? Here is some insight.
What is Yoga Therapy?
Yoga therapy involves a variety of practices that can help ease a natural process or improve a health condition. Some of the therapeutic tools that are used are breathing exercises, physical postures, guided imagery and meditation. Diet is also considered part of yoga therapy.
While regular yoga, depending on the type, can be fast-paced and physically demanding, yoga therapy serves as a safe, gentler alternative. It is led by yoga teachers who are specially trained to work with patients suffering from various health conditions. Just as each patient is different, the styles and formats of yoga therapy also differ greatly. They can vary from small therapeutic classes and one-on-one sessions to chair yoga in nursing homes and hospitals.
Yoga therapy takes a more holistic approach to healing, focusing on patients as a whole instead of just on their conditions. The practice simultaneously works on the body, mind, and spirit, strengthening the body’s different systems. These include the heart and cardiovascular system, muscles, the lungs, as well as the body’s nervous system.
Individuals may suffer from multiple conditions at once, so yoga therapy can be a multi-purpose form of healing. Yoga practices can simultaneously improve digestive system function, nurture psychological well-being, and enhance delivery of oxygen to the body’s tissues. Yoga also can assist the body to more effectively remove carcinogens, waste products and toxins.
Why Is It a Growing Trend?
Yoga therapy is still considered to be a new professional field. However, it is now recognized worldwide as a clinically viable treatment. There are established yoga therapy programs at major health care centers and clinics around the United States. It is increasingly being used regularly in health care facilities and hospitals. As more and more physicians see that yoga therapy helps their patients feel better, it is increasingly becoming a component of medical care.
For the last 12 years, the International Association of Yoga Therapists (IAYT), which has over 3,400 individual members from 48 countries, has worked hard to establish yoga as an esteemed and recognized therapy in the West. It has published an annual peer-reviewed medical journal, presented at academic research conferences, and received an NIH grant to create rigorous yoga therapy certification standards. It is now accrediting training programs and beginning to certify therapist graduates.
The IAYT database of yoga-therapy training programs has grown from five in 2003 to more than 130 schools worldwide today. These include 24 arduous multi-year programs that have been recently accredited by IAYT; there are an additional 20 still under review. As of 2015, most IAYT yoga-therapy practitioners work in hospital settings, while others work in outpatient clinics or physical therapy, oncology, or rehabilitation departments as well as in private practice.
Clinical research is partly responsible for the growing acceptance of yoga therapy in the health care sector. A growing body of research documents the proven benefits of yoga when using it to treat a wide range of health conditions, including anxiety, back pain, insomnia and depression. It is also proven to help reduce risk factors for hypertension and cardiovascular disease. Research also shows that yoga therapy has been successful in alleviating the side effects of cancer treatment. Some patients who have practiced yoga while undergoing radiation therapy have reported lower levels of fatigue, stress and a better quality of life.
Is Yoga Therapy Effective?
Yoga therapy has been proven to be a particularly effective way to reduce stress. This is good news for most people in the West, who encounter high levels of stress on a daily basis. Stress has been known to cause or contribute to varying medical problems, ranging from irritable bowel syndrome, migraine headaches and potentially life-threatening conditions such as heart disease, diabetes and osteoporosis.
When combined with other types of health care, whether alternative or conventional, yoga therapy has proven to be particularly effective, especially in healing chronic ailments. For instance, studies show that in addition to reducing the side effects of chemotherapy and radiation treatments for cancer patients, yoga therapy can also enable faster recovery after bypass surgery. In clinical trials, many patients with high blood pressure, type II diabetes or asthma, who began practicing yoga regularly, were able to lower the lower the dosage of drugs they needed or eliminate some pills entirely. For patients, less medication means fewer side effects, not to mention, greater monetary savings.
The Future of Yoga Therapy
It will still take more time for the practitioners and patients to fully accept yoga therapy as a primary approach to their medical treatment. But even as a supplemental approach, yoga therapy is making great strides. The growing body of scientific research documenting its health benefits is great evidence that yoga therapy is here to stay.
This article originally appeared on huffingtonpost.com and was written by Avital Scharf.
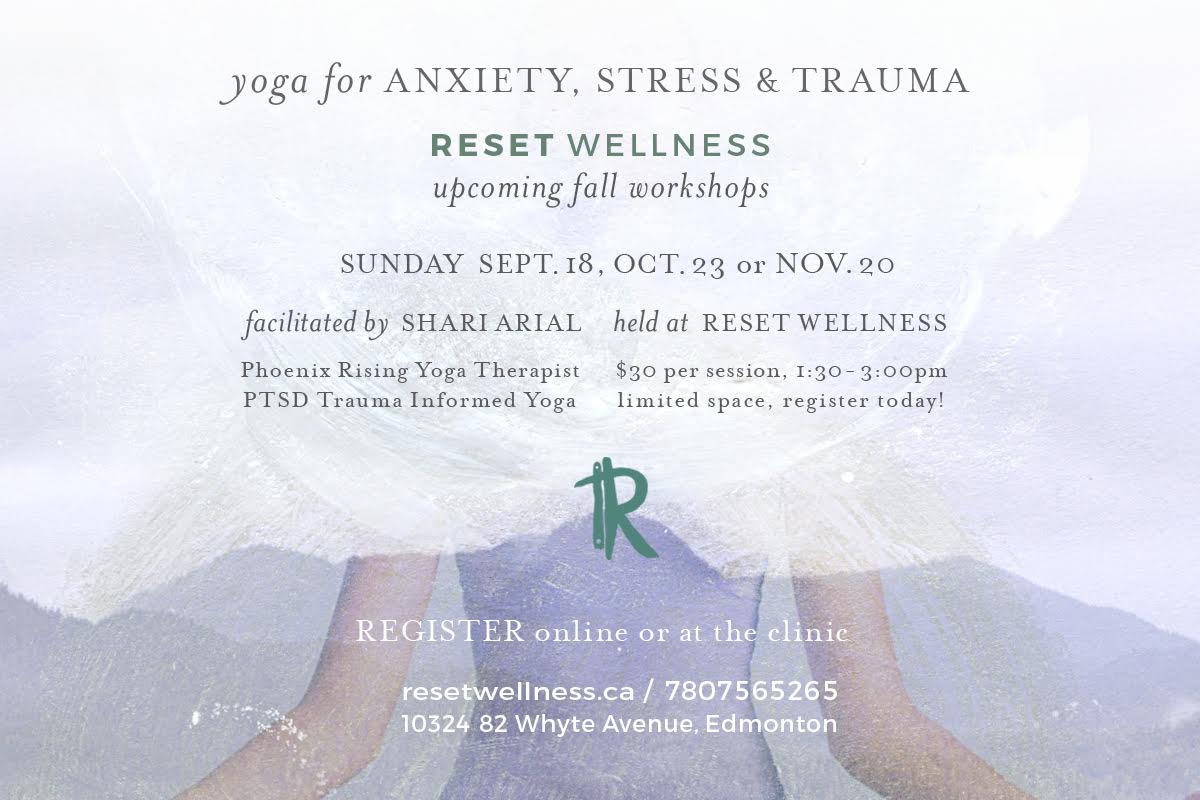
Yoga Therapy services available through Reset Wellness, visit our website for more details.











![Self-regulation “control [of oneself] by oneself"](https://images.squarespace-cdn.com/content/v1/55563e14e4b01769086817cb/1542845645966-PO2HGKF5JLUBM45UIWQ3/wee-lee-790761-unsplash.jpg)